Calcium oxalate urolithiasis
- Components: calcium, oxalate
- Oxalate is metabolised from the amino acid glycine
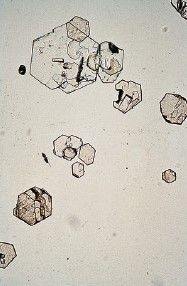
- Two types of calcium oxalate crystals:
- mono-hydrate (dumbbell / oval shape)
- dihydrate (envelope / octahedral shape)


The urine pH does not affect the solubility of Ca-oxalate, but acid urine is associated with increased calcium excretion in the urine
Calcium oxalate can not be dissolved!
The incidence of calcium oxalate increases with age. In dogs, the incidence is higher in males and some breeds (Schnauzers, Terriers, Maltesers, Shih Tzus) are more prone to develop calcium oxalate.
The aetiology of calcium oxalate is still not completely clear, but hypercalciuria seems to play an important role.
Calcium oxalate can form
- At high urinary concentrations of calcium and oxalate
- Especially at low urine pH (associated with increased excretion of calcium in the urine)
- At low concentration of inhibitors (e.g. citrate) or presence of promotors (e.g. uric acid)
Calcium oxalate stone formers often have underlying causes (hypercalcemia, hyperparathyroidism, distal renal tubular acidosis, absorptive hypercalciuria, renal calcium leakage)
Nutritional management of calcium oxalate urolithiasis
As calcium oxalate cannot be dissolved, nutritional management is focused on reduction of recurrence.
- Reduce dietary protein level
- Less intake of glycine which can be metabolised into oxalate
- Protein reduction is associated with reduced urinary calcium and increased urinary citrate concentration
- Urine pH at 6.5-7.5 (to prevent high urinary Ca excretion at low urine pH)
- Low sodium (high sodium intake increases urinary Ca excretion)
- Add potassium citrate (citrate keeps calcium in solution and potassium citrate can increase urine pH)
- Increase urinary volume
A role for omega-3 fatty acids from fish oil (EPA & DHA) in the reduction of recurrence of calcium oxalate?
In a study* with healthy cats, supplementation of a control diet with fatty acids (0.1% arachidonic acid, 0.09% EPA and 0.18% DHA):
- Decreased urine specific gravity, urinary calcium concentration and RSS for struvite
- Increased the resistance to calcium oxalate formation
Also in a review of human studies **, supplementation with polyunsaturated fatty acids, especially EPA and DHA, was frequently associated with reduced urinary calcium and oxalate concentration and it reduced calcium oxalate nephrolith recurrence in a study with stone formers
* Hall JA, Brockman JA, Davidson SJ, MacLeay JM, Jewell DE (2017) Increased dietary long-chain polyunsaturated fatty acids alter serum fatty acid concentrations and lower risk of urine stone formation in cats. PLoS ONE 12(10): e0187133. https://doi.org/10.1371/journal.pone.0187133
** Rodgers AL & Siener R (2020) The efficacy of polyunsaturated fatty acids as protectors against calcium oxalate renal stone formation: a review. Nutrients 2020, 12, 1069; doi:10.3390/nu12041069